By HALEY BRIDGER
Brigham and Women’s/The Harvard Gazette
Heart failure is a common and devastating disorder for which there is no cure. Many conditions that make it difficult for the heart to pump blood—such as dilated cardiomyopathy and arrhythmogenic cardiomyopathy—can lead to heart failure, but treatments for patients with heart failure do not take these distinct conditions into account.
Investigators from Harvard Medical School and Brigham and Women’s Hospital set out to identify molecules and pathways that may contribute to heart failure, with the aim of informing more effective and personalized treatments.
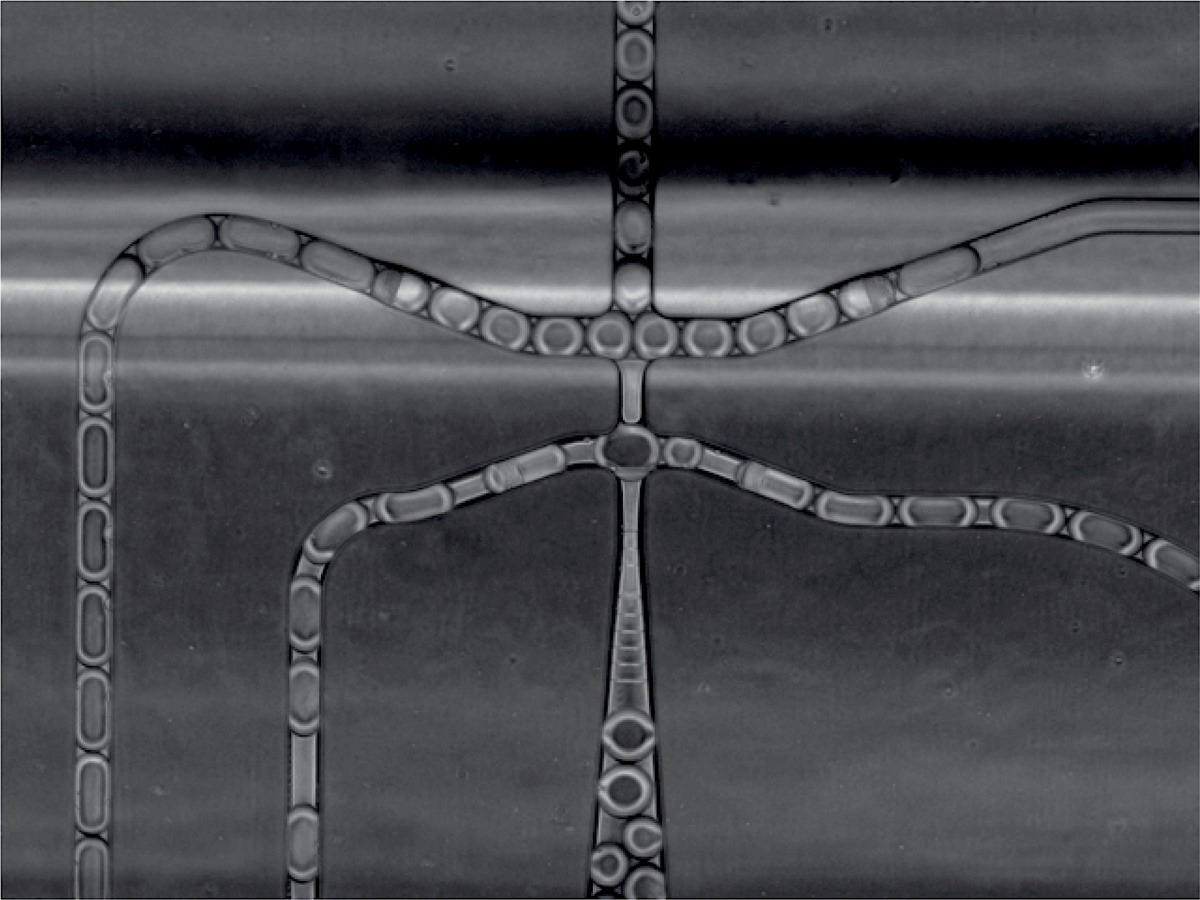
Using single nucleus RNA sequencing, or snRNAseq, to gain insight into the specific changes that occur in different cell types and cell states, the team made several surprising discoveries.
They found that while there are some shared genetic signatures, others are distinct, providing new candidate targets for therapy and predicting that personalized treatment could improve patient care. Results were published online August 4 in Science.
“Our findings hold enormous potential for rethinking how we treat heart failure and point to the importance of understanding its root causes and the mutations that lead to changes that may alter how the heart functions,” said co-senior author Christine Seidman, the Thomas W. Smith Professor of Medicine and professor of genetics in the Blavatnik Institute at HMS and director of the Cardiovascular Genetics Center at Brigham and Women’s.
“This is fundamental research, but it identifies targets that can be experimentally pursued to propel future therapeutics,” she said. “Our findings also point to the importance of genotyping. Not only does genotyping empower research but it can also lead to better, personalized treatment for patients.”
Seidman and Jonathan Seidman, the Henrietta B. and Frederick H. Bugher Foundation Professor of Genetics at HMS, collaborated with an international team.
To conduct their study, the Seidmans and colleagues analyzed samples from 18 control and 61 failing human hearts from patients with dilated cardiomyopathy, arrhythmogenic cardiomyopathy, or an unknown cardiomyopathy disease.
The human heart is composed of many different cell types, including cardiomyocytes (beating heart cells), fibroblasts (which help form connective tissue and contribute to scarring), and smooth muscle cells. The team used single nucleus RNA sequencing to look at the genetic readouts from individual cells and determine cellular and molecular changes in each distinct cell type.
From these data, the team identified 10 major cell types and 71 distinct transcriptional states.
They found that in the tissue from patients with dilated or arrhythmogenic cardiomyopathy, cardiomyocytes were depleted while endothelial and immune cells were increased. Overall, fibroblasts did not increase but showed altered activity.
Analyses of multiple hearts with mutations in certain disease genes—including TTN, PKP2, and LMNA—uncovered molecular and cellular differences as well as some shared responses.