By Tanner Stening
News at Northeastern
With a highly contagious COVID-19 variant spreading rapidly across the U.S., herd immunity—once heralded to be the way out of the pandemic—may no longer be a possibility, several Northeastern experts say.
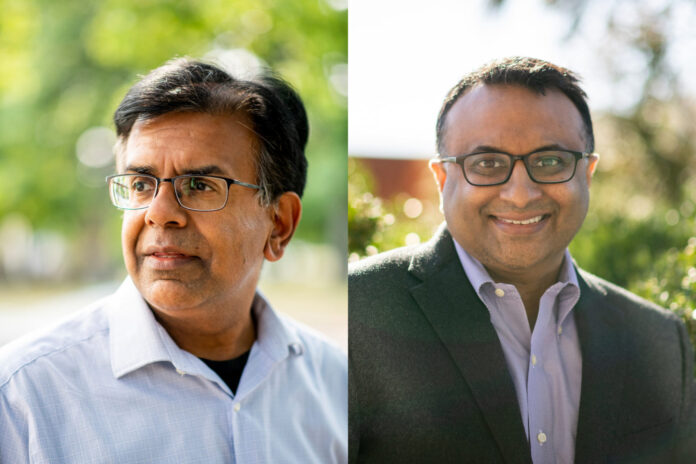
The concept of herd immunity has been offered up by health experts as a largely theoretical but important turning point in the COVID-19 pandemic. But hopes that the U.S. can achieve that critical mass of protection, whether by vaccination or natural infection, has started to wane, largely due to the Delta variant, says Mansoor Amiji, Northeastern University Distinguished Professor in the departments of pharmaceutical sciences and chemical engineering.
“In my opinion, the concept of herd immunity no longer exists,” Amiji says.
Early estimates in 2020 of what percentage of the population would need to be immune from infection to achieve herd immunity hovered between 70 and 80%. But that threshold has since risen, as more infectious variants began circulating.
Now that cases are rising across the country again because of the high transmissibility of the Delta variant, even with more than half of the U.S. population fully vaccinated, it’s time that health authorities rethink the pandemic “endgame,” says Neil Maniar, professor of the practice and director of the Master of Public Health in Urban Health program at Northeastern.
And that means throwing out herd immunity—which has helped inform the vaccine goal posts for cities and towns across the country—as a measure of progress, Maniar says.
“I don’t think herd immunity should be our focus anymore,” Maniar says. “We’re seeing now that even in a largely vaccinated population, you can still have spread, and that challenges one of the key goals of herd immunity.”
The goal now, Maniar says, should be to continue efforts to control infection rates. That means masking and urging that people continue to get the vaccine, which Maniar says “offers a higher degree of protection than natural immunity.”
While the vaccines still offer robust immunity against the Delta variant, they are less effective against the mutation than earlier versions of the coronavirus, Maniar says. Still, the rates of so-called “breakthrough infections” are very low, and communities with higher vaccination rates are seeing less spread—another indication that the vaccines are helping to curb transmission, Maniar says.
But, as Pfizer and Moderna work on vaccine booster shots designed to combat the Delta variant, experts are still trying to understand how long vaccine- or infection-based immunity lasts. Even more concerning is the fact that fully vaccinated people can still pass on the infection to others, even if they don’t become ill themselves, Maniar says.
“It is important that we understand as much as we can about each of these variants, because they’re not going to go away,” he says.
Nationwide, daily cases have been about 10 times higher in recent days than they were in June, and hospitalizations are at their highest point since February. Summertime outbreaks, such as the one in Provincetown, Massachusetts, tied to Fourth of July celebrations there, have provided experts with insight into the transmissibility of the Delta variant, Maniar says.
The speed with which the mutation, which first emerged in India, is taking root in the U.S. is a sign that “we’re facing a new kind of threat,” Maniar says.
“We really can’t let our guard down,” he says, noting that another COVID-19 variant—the Lambda variant—is starting to “vie for the spotlight.”
It also is important that U.S. health authorities continue to expand their thinking about infection control policies beyond the nation’s borders, where several of the highly contagious variants first emerged, Amiji says.
“We really need to be more globally-minded,” Amiji says. “Even if we are very successful in our vaccination program, variants can come from elsewhere and upend that progress.”
And they have. The virus is now “constantly changing,” so much so that it’s making herd immunity an unattainable goal, Amiji says.
“The most important thing at this point is making sure that as many Americans, and as many people across the globe, are vaccinated as possible,” he says.
(Reprinted with permission from the News at Northeastern.)